Optimizing Patient Outcomes With Precision Diagnostics

The modern healthcare landscape is undergoing a monumental shift from a generalized “one-size-fits-all” treatment model to a highly targeted approach known as precision medicine. For decades, medical practitioners were forced to rely on broad symptoms and average population data to make critical decisions about patient care. Today, the integration of advanced diagnostic technologies allows doctors to look deep into the molecular and genetic makeup of an individual to identify the root cause of an illness. This evolution is not just about faster results; it is about the accuracy and the strategic application of data to prevent diseases before they even manifest.
Precision diagnostics act as the vanguard of this movement, providing the essential roadmap for personalized therapies and improved recovery rates. As we move away from reactive medicine, the focus is shifting toward proactive health management powered by high-resolution imaging and biochemical analysis. This article explores the transformative role of these diagnostic tools and how they are fundamentally changing the way we perceive human health. Understanding these systems is vital for anyone looking to navigate the future of global medicine and the incredible possibilities of targeted healing.
The Foundation of Genomic Sequencing and Analysis

At the heart of precision diagnostics lies the ability to map the human genome with incredible speed and decreasing costs. Genomic sequencing allows scientists to identify specific mutations or variations in a person’s DNA that might make them more susceptible to certain cancers or cardiovascular issues.
By understanding the genetic blueprint, clinicians can predict how a patient will respond to specific medications, a field known as pharmacogenomics. This prevents the dangerous “trial and error” phase of prescribing drugs that might cause adverse reactions. Genomic data provides a baseline for lifelong health monitoring that is unique to every single human being.
A. Whole Genome Sequencing (WGS)
This process involves analyzing the entire DNA sequence of an individual to find rare genetic disorders or complex disease markers. It is the most comprehensive form of genetic testing available and serves as a permanent reference for a patient’s medical history.
B. Targeted Gene Panels
For patients with a family history of specific conditions, targeted panels focus on a smaller group of genes known to be associated with those risks. This is a faster and more cost-effective way to get high-impact results for conditions like hereditary breast cancer or Lynch syndrome.
C. Pharmacogenomic Testing
This specialized branch of diagnostics studies how genes affect a person’s response to drugs. It helps doctors choose the exact right dosage and the specific type of medication that will be most effective for the patient’s unique metabolism.
Artificial Intelligence in Medical Imaging
Medical imaging has progressed far beyond the standard X-ray to include high-resolution MRI, CT scans, and PET scans that produce massive amounts of data. Human radiologists are now being supported by Artificial Intelligence (AI) algorithms that can spot microscopic abnormalities that the naked eye might miss.
These AI systems are trained on millions of previous cases, allowing them to provide a “second opinion” with incredible statistical backing. This reduces the rate of false negatives and ensures that diseases like early-stage lung cancer are caught when they are most treatable. AI doesn’t replace the doctor; it provides them with a “super-vision” that enhances their diagnostic accuracy.
A. Automated Lesion Detection
AI software can scan thousands of images in seconds to identify suspicious growths or lesions in organs like the liver or brain. This speed is critical in emergency rooms where every second counts for stroke or trauma victims.
B. Predictive Analytics for Disease Progression
By comparing current scans with historical data, AI can predict how a disease is likely to spread or respond to treatment. This allows oncologists to adjust chemotherapy or radiation plans in real-time based on the actual behavior of a tumor.
C. Image Enhancement and Noise Reduction
Advanced software can clean up “grainy” images from older machines or low-dose radiation scans. This provides a clearer picture for the surgeon while reducing the patient’s overall exposure to harmful radiation.
The Evolution of Liquid Biopsies
Traditional tissue biopsies are invasive, painful, and sometimes carry significant risks depending on the location of the tumor. Liquid biopsies represent a breakthrough in precision diagnostics by allowing doctors to detect cancer markers through a simple blood draw. These tests look for “circulating tumor DNA” (ctDNA) shed by cancerous cells into the bloodstream.
This allows for constant monitoring of a patient’s condition without the need for repeated surgeries. Liquid biopsies are becoming an essential tool for early detection and for tracking how well a patient is responding to immunotherapy.
A. Early Cancer Screening
Liquid biopsies can detect signs of cancer months or even years before a physical tumor appears on an imaging scan. This “early warning system” is the holy grail of oncology, as it significantly increases the chances of a full cure.
B. Monitoring Treatment Resistance
Cancers are constantly evolving, and a treatment that worked yesterday might not work tomorrow. Liquid biopsies allow doctors to see if a tumor has developed new mutations that make it resistant to current drugs, allowing for an immediate shift in strategy.
C. Minimal Residual Disease (MRD) Testing
After surgery or chemotherapy, MRD tests check if any microscopic cancer cells are still hiding in the blood. This helps determine if a patient needs additional “mop-up” treatment or if they can safely enter a period of observation.
Remote Patient Monitoring and Wearable Sensors
Precision diagnostics are moving out of the hospital and into the daily lives of patients through wearable technology. Smartwatches and specialized patches can now monitor heart rate, blood oxygen levels, and even glucose levels continuously. This “real-world” data provides a much more accurate picture of a patient’s health than a single 15-minute appointment in a doctor’s office.
For patients with chronic conditions like diabetes or heart failure, these devices can send an alert to their medical team before a crisis occurs. This creates a continuous loop of data that allows for truly personalized and immediate care.
A. Continuous Glucose Monitors (CGM)
For diabetics, CGMs eliminate the need for constant finger-pricking by providing a constant stream of sugar level data to a smartphone. The system can even talk to an insulin pump to automatically adjust doses, mimicking a healthy pancreas.
B. Wearable ECG and Heart Rhythm Tracking
Wearables can now detect atrial fibrillation (AFib) and other irregular heart rhythms during a patient’s normal daily activities. This data is vital for preventing strokes and managing long-term cardiovascular health without hospitalizing the patient for observation.
C. Smart Inhalers and Respiratory Monitoring
For asthma or COPD patients, sensors on inhalers can track how often a patient needs “rescue” medication and what environmental factors might be triggering their attacks. This allows for a more targeted approach to managing respiratory health.
Point-of-Care Testing (POCT) Innovations
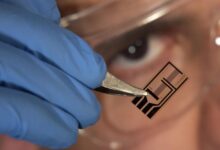
The speed of a diagnosis is often as important as its accuracy, which is where Point-of-Care Testing (POCT) comes in. These are portable diagnostic devices that can provide lab-quality results in a doctor’s office, a pharmacy, or even a remote village. By removing the need to send samples to a centralized lab, POCT significantly reduces the time it takes to start a life-saving treatment.
Modern POCT devices use microfluidics and “lab-on-a-chip” technology to perform complex biochemical assays in minutes. This decentralization of diagnostics is essential for managing infectious diseases and improving health equity globally.
A. Rapid Molecular Diagnostics for Viruses
Devices that use PCR-like technology in a portable format can identify viruses like influenza or COVID-19 with extreme precision. This allows for immediate isolation and treatment, preventing the spread of the virus within the community.
B. Portable Blood Gas and Electrolyte Analyzers
In critical care situations, knowing a patient’s blood pH or potassium levels can be the difference between life and death. POCT devices allow paramedics and ER nurses to get these results at the bedside in less than two minutes.
C. Home-Based Diagnostic Kits
The next generation of POCT includes kits that allow patients to test for strep throat or urinary tract infections at home. The results are then shared with a doctor via a telehealth app for an immediate prescription, saving the patient a trip to the clinic.
Integration of Multi-Omics for Holistic Health
While genomics looks at DNA, other “omics” fields look at different layers of biological information. Proteomics studies the proteins in our body, while metabolomics looks at the chemical fingerprints left by cellular processes. Integrating all this data into a “multi-omics” profile provides the most complete picture of human health ever achieved.
This allows doctors to see not just the genetic potential for a disease, but the actual activity happening in the body at that exact moment. This holistic view is the ultimate expression of precision diagnostics, moving beyond single biomarkers to understand the entire biological system.
A. Proteomic Profiling for Early Disease
Changes in protein levels often occur long before physical symptoms appear. By tracking thousands of proteins simultaneously, researchers can find early markers for Alzheimer’s or autoimmune diseases.
B. Metabolomic Fingerprinting
Our metabolism changes in response to diet, environment, and illness. Mapping these metabolic shifts helps doctors understand the functional state of a patient’s organs and how they are coping with stress or infection.
C. The Microbiome and Gut Health
The trillions of bacteria living in our gut play a massive role in our immune system and mental health. Diagnostics that analyze the microbiome are opening new doors for treating everything from IBS to depression through personalized nutrition and probiotics.
Conclusion

Precision diagnostics represent the most significant leap forward in medical science in our lifetime. The ability to look at a patient’s unique genetic code has removed the guesswork from modern treatment. AI and machine learning are now providing doctors with the tools to spot diseases at an invisible stage. Invasive procedures are being replaced by simple and painless blood tests that provide more data. Wearable technology has turned our daily lives into a continuous stream of vital health information.
The speed of decentralized testing is saving lives by providing results in minutes rather than days. Looking at the whole person through multi-omics is the future of preventative healthcare globally. These technologies are making medicine more proactive and far more effective for every individual. The cost of these advanced tools continues to drop, making them accessible to more people every year. We are finally entering an era where the treatment is as unique as the patient receiving it.